There is a plethora of misinformation and pseudoscientific messages online and in social media platforms. This can make it difficult to understand what the right thing is to do or not do. This article will break down the current scientific and clinical understanding of strength training and the pelvic floor. First, we will discuss what the pelvic floor is and what it does. The we will look at signs of a dysfunctional pelvic floor and what to do about it. Lastly, we will specifically focus on strength training and what it means for the pelvic floor.
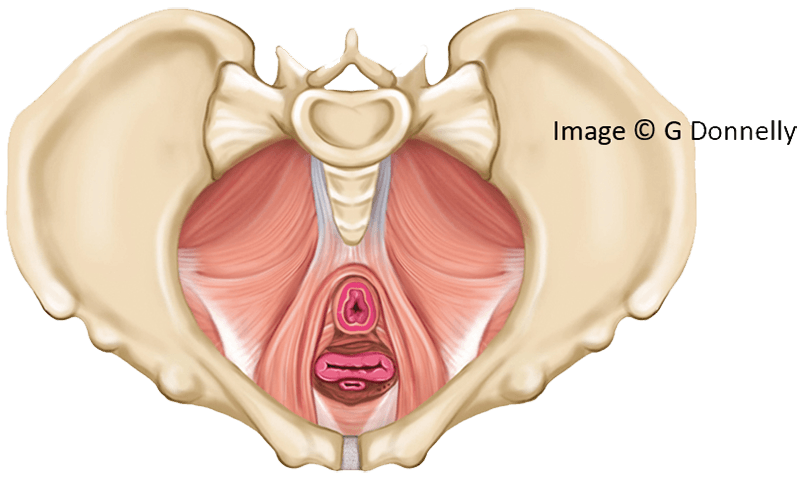
What is the Pelvic Floor?
First and foremost, the female pelvic floor is an incredibly important muscle group. It represents a group of muscle spanning the base of the pelvic outlet in layers with its attachments suspended around the bony perimeter of the pelvis and not one, not two but three intersections compromising it in the form of the urethral, vaginal and rectal openings. It serves to support the pelvic organs, facilitate bladder and bowel control and emptying, and facilitate reproduction. I like to think of the pelvic floor as a trampoline, a structure that needs to be flexible enough to accept and absorb load with enough integrity and strength to give back and respond. Therefore, if the pelvic floor “trampoline” is too stiff, too lax or compromised in its attachments around the perimeter, it may not function as intended.
What are the signs and symptoms of Pelvic Floor Dysfunction?
If the pelvic floor is not functioning as intended, any and all of the roles it is involved in can be compromised (Donnelly and Moore 2022). These include:
- Urinary frequency, urgency and or incontinence
- Bowel frequency, urgency or incontinence
- Difficulty emptying the bladder or bowel fully
- Straining to empty the bowel
- Heaviness, pressure or dragging in the vaginal area
- Pain anywhere in the saddle region or “inside”
- Recurrent urinary tract infections
- Pain with intercourse
- Inability to tolerate intravaginal products e.g., tampons, menstrual cups, smear tests
The presence of one or more of these signs and symptoms need not scare you – across the female lifespan they are actually very common. At least 1 in 3 women will leak from the bladder (Lawrence et al, 2008; Sims et al, 2022) and 1 in 2 women will experience pelvic organ descent (with varying degrees of awareness and symptoms) (Donnelly and Moore 2022). However, they are not to be accepted or suffered either. Like any sports related niggle or injury, we address the presenting symptoms and rehabilitate the driving area. Did you know that there is a dedicated specialist physiotherapy profession who solely deal with pelvic floor dysfunction. That’s right – that is how many people need pelvic floor rehabilitation.
Why might strength training influence symptoms of pelvic floor dysfunction?
Firstly, strength training is not harmful or risky. It is a fundamental component of staying strong and protecting muscle mass and bone density throughout the lifespan. This includes the beneficial effect that strength training will have on building pelvic floor muscle strength and endurance as it trains to meet the demands of the load placed upon it. However, like any area in the body, the level of resistance that we can tolerate depends on the load capacity of the tissues (Gabbett, 2023). This means that while you may be ready to lift a certain barbell weight or kettlebell in terms of your lower limb, upper limb or trunk strength, you may not have the necessary load tolerance in the pelvic floor. This will ultimately lead to exposing symptoms of pelvic floor dysfunction on a lift/exertion. Just like you strengthen the other muscle groups around the body so that you can progress your deadlifts or bench press or any other strength training exercise, you need to engage in targeted strengthening for the pelvic floor too. For some women, it isn’t so much that their pelvic floor is weak or lacking structural integrity - it could be more to do with the strategy they employ during resistance training. For example, some women breath hold and brace their abdominal wall and trunk in order to lift heavy. This bracing and breath hold places additional load and abdominal pressure down onto the pelvic floor (Prevett and Moore 2024). This may be enough to tip the balance from being able to tolerate the load to not being able to tolerate it with signs of load intolerance represented in symptoms such as pain, leaking urine or a heaviness or bulge sensation in the vaginal region. Altering strategies to try to “blow as you go” (breath out of the effort of the strength exercise) or brace the abdominal muscles less intensely may be enough to reduce or alleviate symptoms. Check out this podcast for more information on resistance training and the pelvic floor.
What should I do if I have signs and symptoms of pelvic floor dysfunction?
You can speak with you GP or primary care physician to ask for a referral to your local pelvic health specialist or if you prefer to access healthcare privately there will be a local private pelvic health physiotherapist in your region. Generally speaking, most people benefit from engaging in pelvic floor muscle training – the difficulty is that it can be hard for everyone to know how to do them. If you are unsure they best option is to get assessed and access guidance from a specialist physiotherapist – however typical cues to locate and train the pelvic floor include:
- Imagine you are stopping wind escaping from the back passage
- Imagine stopping the flow of urine mid-flow
- Imagine closing a zip from back passage to front passage
- Close the vagina
No one cue suits everybody therefore consider the cues above and whether you feel a tightening and lifting in the pelvic floor region. It isn’t clenching your glute muscles or squeezing your legs together, it is specifically the muscles in and around the saddle region. Aim to do 3 sets of 8-12 repetitions of close to maximum contractions (Donnelly and Moore 2022). For women who wish to continue strength training while they seek help and rehabilitate their pelvic floor, or after they have reached their rehabilitation potential, several adjunctive products can help with pelvic floor function and support (Giagio and Donnelly 2025). These include compression shorts – which direct compression up towards the pelvic floor. I am researching these in my PhD and they are showing significance in mechanical support, symptom reduction and user perception. Other adjuncts include pessaries (which support the pelvic organs), urethral support devices (support the urethra/bladder) and vaginal weights which can help you progress pelvic floor muscle strengthening.
References
Donnelly GM, Moore IS. Sports Medicine and the Pelvic Floor. Curr Sports Med Rep. 2023 Mar 1;22(3):82-90. doi: 10.1249/JSR.0000000000001045. PMID: 36866951(.
Gabbett T. Load Management: What It Is and What It Is Not! Sports Health. 2023;15(4):478. doi:10.1177/19417381231179946
Giagio S, Salvioli S, Innocenti T, et al PFD-SENTINEL: Development of a screening tool for pelvic floor dysfunction in female athletes through an international Delphi consensus British Journal of Sports Medicine 2023;57:899-905.
Giagio, Silvia PhD1,2; Donnelly, Gráinne M.3. Persistent Pelvic Floor Dysfunction in Female Athletes: A Commentary on Postconservative Management. Current Sports Medicine Reports 24(3):p 65-73, March 2025. | DOI: 10.1249/JSR.0000000000001235
Lawrence JM, Lukacz ES, Nager CW, Hsu JW, Luber KM. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet Gynecol. 2008 Mar;111(3):678-85. doi: 10.1097/AOG.0b013e3181660c1b. PMID: 18310371.
Prevett C. & Moore R. (2024) Nuances of the Valsalva manoeuvre and bracing with regard to resistance training performance and its effects on the pelvic floor. Journal of Pelvic, Obstetric and Gynaecological Physiotherapy 134 (Spring), 31–41.
Sims L, Hay-Smith J, Dean S. Pelvic floor exercises and female stress urinary incontinence. Br J Gen Pract. 2022 Mar 31;72(717):185-187. doi: 10.3399/bjgp22X719033. PMID: 35361602; PMCID: PMC8966921.