Why wasn’t my life worth saving? Is a question that rattles around in my mind a lot.
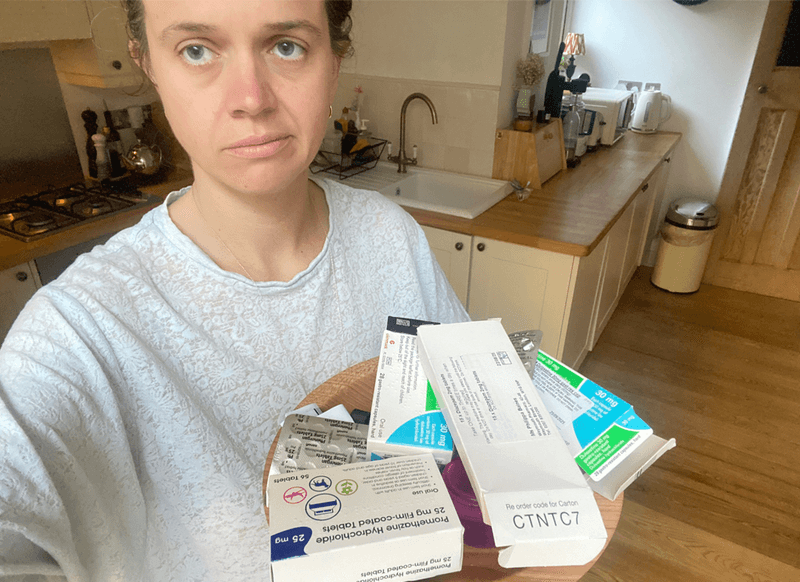
In October 2022, I had my 10th thrush infection.
It was drug-resistant.
Lasted 2 months and gave me nerve damage of the vulva.
I now live with a burning feeling in my genitals 24/7. The level of pain averages out at 6/10 and my career dreams are over, along with my hope for having a baby and starting a family.
Almost daily, I regret being born. Specifically, being born a woman.
They’ve known a severe thrush infection causes vulval nerve damage for quite some time.
‘They’ being The British Association of Dermatologists, who list thrush as a trigger event for ‘vulvodynia’: ‘Secondary vulvodynia may follow inflammation in the vulva, such as that caused by thrush or the overuse of topical and vaginal anti-thrush treatments.’
And the Vulval Pain Society knows, to quote: “a commonly recognised event is a severe attack of thrush followed by anti-thrush treatment. Once the attack of thrush settles following treatment, soreness and burning may persist as vestibulodynia.”
It was also listed as a predisposing factor to developing vestibulodynia in the 2015 meeting on the definition of vulvodynia held by ISSVD, ISSWSH and the IPPS – ‘Some women …have a genetic predisposition to developing this condition …: genetic polymorphisms that increase the risk of candidiasis”
And so I sit here holding an ice pack to my groin and wonder – why no prevention strategy?
Why no warning to women prone to thrush before the nerve damage develops?
Two sentences on the NHS website warning of the link could have saved my life. Here is what I’m suggesting:
“There is an association between thrush and vulval nerve damage, a chronic pain condition called vulvodynia. Women prone to thrush should take all reasonable measures to bring their rate down and consult a vulval clinic if they have any concerns.”
This could have saved my life.
As I could have taken my thrush predisposition seriously.
I wouldn’t have had the coil fitted, which significantly increases your risk of thrush (Marcos et al 2010).
I could have stopped drinking beer, which was a known trigger for me.
I could have gone immediately to a vulval clinic when the thrush lasted more than two weeks.
And they’d have been able to help me tackle the infection using treatments sensitive to the nerve-packed vulval vestibule.
The current guidelines to treat severe thrush with clotrimazole pessary after cloterimazole pessary after clotrimazole pessary (14 to be precise), irritates the vestibule even further according to the British Association of Dermatologists. So why haven’t they updated the guidelines?
When the pain first started for me, I made a full recovery. From October 2022 to March 2023 - my nerves calmed down and I got better.
But because I was never diagnosed, as I was never referred to a vulval clinic. My GP didn’t know they existed and the GUM clinic where I was being cared for said the waitlist was so long for gynaecology departments that there was no point in going to see them if I was improving anyway.
And indeed gynaecologists aren’t taught about the vulva. So they wouldn’t have helped.
Despite 51% of the population having a vulva, vulval pain syndromes are seen as a niche speciality within medicine.
Despite 1 in 4 women developing vulvodynia in a lifetime, only vulval clinics have any understanding of the vulval tissues. The nerve-packed hormone-dependent vestibule that gets irritated so easily, located at the entrance of the vagina.
Medicine should serve the needs of the population.
But women are let so severely down.
Thrush is not something that pharmacists should roll their eyes at.
But a condition that can cause disability via chronic pain.
And can increase a woman’s chance of suicide by over 300% due to the impact of chronic pain.
In the absence of any medical entity wanting to drive change and protect women’s lives - I set up www.thrush-support.com.
A resource hub to help thrush-prone women bring down their rates and get to the right doctors in time to stop nerve damage before it starts.
I raise awareness on Instagram and TikTok - my ‘Story’ post alone has garnered just under 2M views.
Despite this, I’ve had no Doctors or governmental health bodies approach me saying – we really should be doing something about this. Let’s collaborate.
Every woman’s life is worth safeguarding. And that starts with taking their health issues seriously. And listening to their voices.
I thank Women’s Health Pathway for really appreciating the magnitude of this issue and allowing me this platform to warn others.
No woman should be made disabled by a thrush infection.
Every woman’s life is worth saving.